
DIAGNOSING HEEL PAIN AND PLANTAR FASCIITIS
Heel pain is most often caused by Plantar Fasciitis, a condition that is sometimes also called heel spur syndrome when a spur is present. Heel pain may also be due to other causes, such as a stress fracture, tendonitis, arthritis, nerve irritation, or, rarely, a cyst.

WHAT IS PLANTAR FASCIITIS?
Because there are several potential causes, it is important to have heel pain properly diagnosed. A foot and ankle surgeon is able to distinguish between all the possibilities and determine the underlying source of your heel pain. Plantar Fasciitis is an inflammation of the band of tissue (the plantar fascia) that extends from the heel to the toes. In this condition, the fascia first becomes irritated and then inflamed, resulting in heel pain.
HEEL PAIN CAUSES
The most common cause of Plantar Fasciitis relates to faulty structure of the foot. For example, people who have problems with their arches, either overly flat feet or high-arched feet, are more prone to developing Plantar Fasciitis.
Wearing non-supportive footwear on hard, flat surfaces puts abnormal strain on the Plantar Fascia and can also lead to Plantar Fasciitis. This is particularly evident when one’s job requires long hours on the feet. Obesity may also contribute to Plantar Fasciitis.

DIAGNOSING HEEL PAIN AND PLANTAR FASCIITIS
Heel pain is most often caused by Plantar Fasciitis, a condition that is sometimes also called heel spur syndrome when a spur is present. Heel pain may also be due to other causes, such as a stress fracture, tendonitis, arthritis, nerve irritation, or, rarely, a cyst.

WHAT IS PLANTAR FASCIITIS?
Because there are several potential causes, it is important to have heel pain properly diagnosed. A foot and ankle surgeon is able to distinguish between all the possibilities and determine the underlying source of your heel pain. Plantar Fasciitis is an inflammation of the band of tissue (the plantar fascia) that extends from the heel to the toes. In this condition, the fascia first becomes irritated and then inflamed, resulting in heel pain.
HEEL PAIN CAUSES
The most common cause of Plantar Fasciitis relates to faulty structure of the foot. For example, people who have problems with their arches, either overly flat feet or high-arched feet, are more prone to developing Plantar Fasciitis.
Wearing non-supportive footwear on hard, flat surfaces puts abnormal strain on the Plantar Fascia and can also lead to Plantar Fasciitis. This is particularly evident when one’s job requires long hours on the feet. Obesity may also contribute to Plantar Fasciitis.
HEEL PAIN SYMPTOMS & DIAGNOSIS
SYMPTOMS
The symptoms of Plantar Fasciitis are:
- Pain on the bottom of the heel (stabbing Pain)
- Pain that is usually worse upon waking up, arising
- Pain that increases over a period of months
People with Plantar Fasciitis often describe the pain as worse when they get up in the morning or after they’ve been sitting for long periods of time. After a few minutes of walking the pain decreases, because walking stretches the fascia. For some people the pain subsides but returns after spending long periods of time on their feet.
DIAGNOSIS
To arrive at a diagnosis, the foot and ankle surgeon will obtain your medical history and examine your foot. Throughout this process the surgeon rules out all the possible causes for your heel pain other than plantar Fasciitis.
In addition, diagnostic imaging studies such as x-rays or other imaging modalities may be used to distinguish the different types of heel pain. Sometimes heel spurs are found in patients with Plantar Fasciitis, but these are rarely a source of pain. When they are present, the condition may be diagnosed as Plantar Fasciitis/heel spur syndrome.
NON-SURGICAL TREAMENT FOR PLANTAR FASCIITIS
STRETCHING EXERCISES
Exercises that stretch out the calf muscles help ease pain and assist with recovery. Avoid going barefoot. When you walk without shoes, you put undue strain and stress on your plantar fascia.
Ice. Putting an ice pack on your heel for 20 minutes several times a day helps reduce inflammation. Place a thin towel between the ice and your heel; do not apply ice directly to the skin.
Limit activities. Cut down on extended physical activities to give your heel a rest. Shoe modifications. Wearing supportive shoes that have good arch support and a slightly raised heel reduces stress on the plantar fascia.
Medications. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be recommended to reduce pain and inflammation.
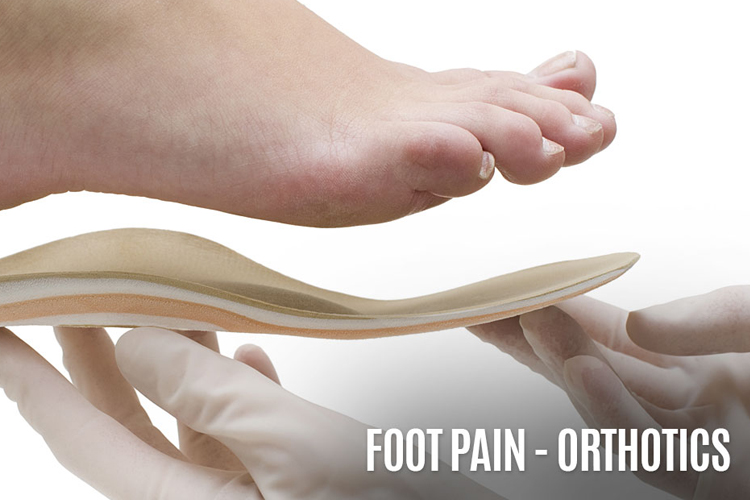
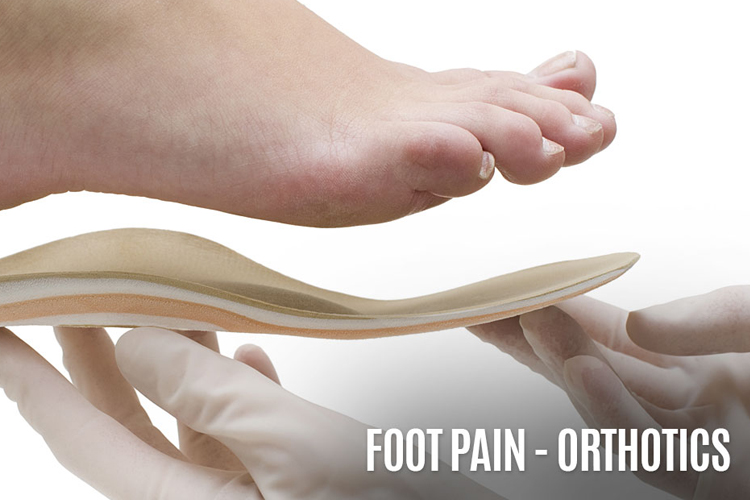
PADDING & STRAPPING
Placing pads in the shoe softens the impact of walking. Strapping helps support the foot and reduce strain on the fascia.
Orthotic devices. Custom orthotic devices that fit into your shoe help correct the underlying structural abnormalities causing the Plantar Fasciitis. Injection therapy. In some cases, corticosteroid injections are used to help reduce the inflammation and relieve pain.
Removable walking cast. A removable walking cast may be used to keep your foot immobile for a few weeks to allow it to rest and heal.
Night splint. Wearing a night splint allows you to maintain an extended stretch of the plantar fascia while sleeping. This may help reduce the morning pain experienced by some patients.
Physical therapy. Exercises and other physical therapy measures may be used to help provide relief.

WHEN IS SURGERY NEEDED?
Although most patients with Plantar Fasciitis respond to non-surgical treatment, a small percentage of patients may require surgery. If, after several months of non-surgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you.
LONG-TERM CARE
No matter what kind of treatment you undergo for Plantar Fasciitis, the underlying causes that led to this condition may remain. Therefore, you will need to continue with preventive measures. Wearing supportive shoes, stretching, and using custom orthotic devices are the mainstay of long-term treatment for Plantar Fasciitis.
ORTHOTICS & SPECIAL INSERTS
Do you need special padding in your shoes to support your feet? Orthotics can lend relief and could be the immediate answer. Visit our Orthotics page for other related foot and ankle pain. If you are a resident of the LA, San Diego, Riverside, San Bernardino or Orange County area, you can benefit from our services.

WHEN IS SURGERY NEEDED?
Although most patients with Plantar Fasciitis respond to non-surgical treatment, a small percentage of patients may require surgery. If, after several months of non-surgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you.
LONG-TERM CARE
No matter what kind of treatment you undergo for Plantar Fasciitis, the underlying causes that led to this condition may remain. Therefore, you will need to continue with preventive measures. Wearing supportive shoes, stretching, and using custom orthotic devices are the mainstay of long-term treatment for Plantar Fasciitis.
ORTHOTICS & SPECIAL INSERTS
Do you need special padding in your shoes to support your feet? Orthotics can lend relief and could be the immediate answer. Visit our Orthotics page for other related foot and ankle pain. If you are a resident of the LA, San Diego, Riverside, San Bernardino or Orange County area, you can benefit from our services.

